Table of Contents
Welcome to the intricate realm of metabolic control, where a modest yet mighty organ plays a pivotal role in regulating our body’s sugar levels—the pancreas. Nestled behind the stomach, this unassuming gland carries the responsibility of producing vital hormones and enzymes essential for digestion and maintaining blood glucose balance. Join us on an enlightening journey into the complexities of pancreatic anatomy, function, and the profound impact it has on overall health. This page is your gateway to unravelling the mysteries of the pancreas—a silent orchestrator behind the scenes, influencing our daily metabolic dance.
ANATOMY

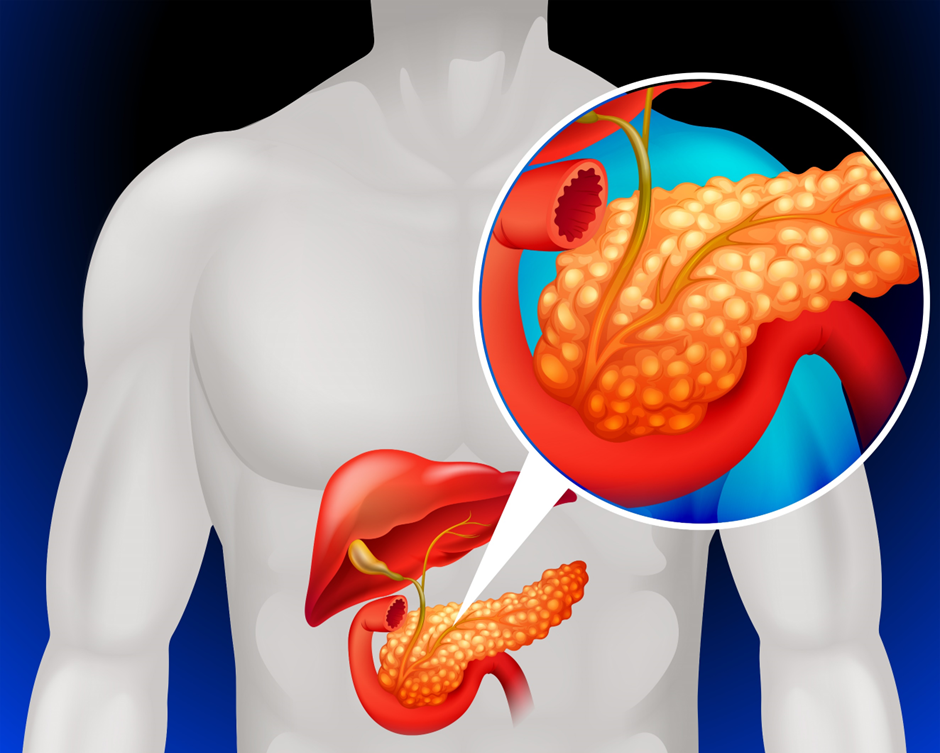
The pancreas is a dual-function organ with both endocrine and exocrine functions, situated behind the stomach in the abdominal cavity. Let’s delve into the key components of its anatomy:
HEAD
The head of the pancreas is a crucial anatomical region that constitutes the rightmost part of this organ. Located near the curve of the duodenum (the first part of the small intestine), the head of the organ is vital for digestive processes. This region serves as the starting point for the main pancreatic duct, which transports digestive enzymes to the duodenum, aiding in the breakdown of food. Additionally, the head of the pancreas plays a key role in the endocrine function, hosting clusters of cells known as islets of Langerhans that produce insulin and other hormones.
BODY
The body of the pancreas is a central and elongated portion of this vital organ, lying behind the stomach. Positioned horizontally, it connects the head of the pancreas on the right side to the tail on the left side. The body of the pancreas is integral to the organ’s dual functionality, housing both endocrine and exocrine cells. Within the islets of Langerhans in this region, beta cells produce insulin, a hormone crucial for blood sugar regulation. Simultaneously, exocrine cells in the pancreatic body generate digestive enzymes essential for breaking down nutrients in the small intestine.
TAIL
The tail of the pancreas is the elongated and tapering end of this vital organ, extending towards the left side of the abdomen. While the tail is structurally connected to the body of the pancreas, it narrows as it approaches the spleen. The tail is a critical region for the pancreas’s endocrine and exocrine functions. It contains islets of Langerhans, where alpha, beta, and delta cells contribute to the regulation of blood sugar through the production of insulin, glucagon, and somatostatin. Additionally, the tail of the organ continues the exocrine function by releasing digestive enzymes into the small intestine.
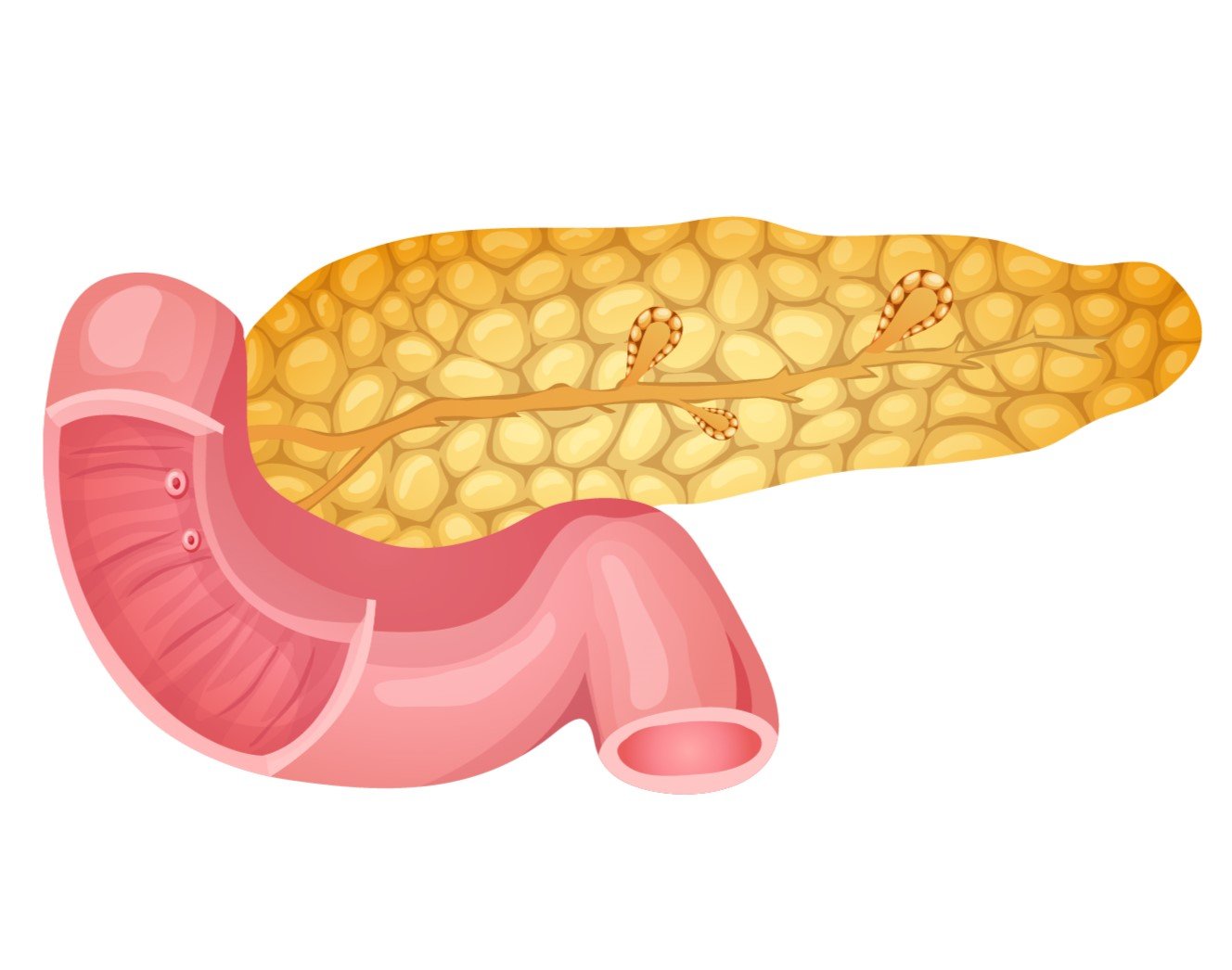
PANCREATIC DUCTS
- Main Pancreatic Duct: Extending through the entire length of the pancreas, the main pancreatic duct carries digestive enzymes produced by the exocrine cells to the duodenum.
- Accessory Pancreatic Duct: A smaller duct that also connects to the duodenum, providing an alternative route for pancreatic secretions.
ISLETS OF LANGERHANS
These are clusters of cells scattered throughout the pancreas responsible for its endocrine function. The islets contain different cell types, including:
- Alpha Cells: Produce glucagon, a hormone that raises blood sugar levels.
- Beta Cells: Produce insulin, a hormone that lowers blood sugar levels.
- Delta Cells: Produce somatostatin, which regulates the release of insulin and glucagon.
EXOCRINE CELLS
The majority of the pancreas consists of exocrine tissue, which produces digestive enzymes that aid in the breakdown of food in the small intestine. The enzymes include amylase, lipase, and proteases.
BLOOD VESSELS
The pancreas is a well-vascularized organ with a network of blood vessels that ensures its proper functioning. The blood vessels of the pancreas supply oxygen and nutrients to the various cells within the organ. The key blood vessels associated with the pancreas include:
- Pancreatic Arteries: The pancreatic arteries, branches of the celiac artery, supply oxygenated blood to the pancreas. These arteries further divide into smaller vessels to reach different parts of the organ.
- Splenic Artery: The splenic artery, arising from the celiac artery, provides blood supply to the spleen, and some of its branches extend to the tail of the pancreas.
- Superior Mesenteric Artery: The superior mesenteric artery, another branch of the abdominal aorta, contributes to the blood supply of the pancreas, particularly to the head and part of the body.
- Pancreatic Veins: Blood is drained from the pancreas through a network of veins, ultimately forming the pancreatic veins. These veins carry deoxygenated blood away from the pancreas, and they usually join the portal vein, which transports blood to the liver.
FUNCTION
The pancreas is a multifunctional organ with both endocrine and exocrine functions, contributing to crucial processes in the body. Here are the key functions of the pancreas:
ENDOCRINE FUNCTION
- Insulin Production (Beta Cells): Beta cells in the islets of Langerhans produce insulin, a hormone that plays a central role in regulating blood sugar (glucose) levels. Insulin facilitates the uptake of glucose by cells for energy or storage in the liver and muscles.
- Glucagon Production (Alpha Cells): Alpha cells in the islets of Langerhans produce glucagon, a hormone that stimulates the release of glucose from the liver into the bloodstream. This helps raise blood sugar levels when needed.
- Somatostatin Production (Delta Cells): Delta cells produce somatostatin, a hormone that regulates the release of insulin and glucagon, helping to maintain balanced blood sugar levels.
EXOCRINE FUNCTION
- Enzyme Production: The exocrine cells of the pancreas produce digestive enzymes essential for breaking down macronutrients in the small intestine. These enzymes include:
- Amylase: Breaks down carbohydrates (starches) into sugars.
- Lipase: Breaks down fats into fatty acids and glycerol.
- Proteases (Trypsin, Chymotrypsin): Break down proteins into amino acids.
- Bicarbonate Production: The pancreas secretes bicarbonate, an alkaline substance that neutralizes the acidic chyme (partially digested food) entering the small intestine from the stomach. This creates an optimal pH environment for the activity of digestive enzymes.
REGULATION
- Metabolic Regulation: The pancreas plays a crucial role in overall metabolic regulation, influencing energy balance and nutrient utilization in the body.
- Blood Sugar Regulation: The insulin and glucagon hormones work in tandem to regulate blood sugar levels, ensuring a balance between glucose uptake by cells and glucose release from the liver.
SECRETION CONTROL
The pancreas tightly regulates the secretion of insulin and other hormones in response to changes in blood glucose levels, dietary intake, and metabolic demands.
HORMONAL COORDINATION
The endocrine hormones produced by the pancreas act in coordination with hormones from other glands to maintain homeostasis and respond to varying physiological conditions.
DISEASES
The pancreas is susceptible to various diseases that can impact its endocrine and exocrine functions. Here are some common diseases associated with the pancreas:
- Diabetes Mellitus:
- Type 1 Diabetes: An autoimmune condition where the immune system attacks and destroys the insulin-producing beta cells in the pancreas.
- Type 2 Diabetes: Characterized by insulin resistance, where cells do not respond effectively to insulin. Over time, the pancreas may also fail to produce enough insulin.
- Pancreatitis:
- Acute Pancreatitis: Inflammation of the pancreas, often caused by gallstones or excessive alcohol consumption. Symptoms include severe abdominal pain, nausea, and vomiting.
- Chronic Pancreatitis: Ongoing inflammation that leads to permanent damage to the pancreas. It can result in digestive issues and diabetes.
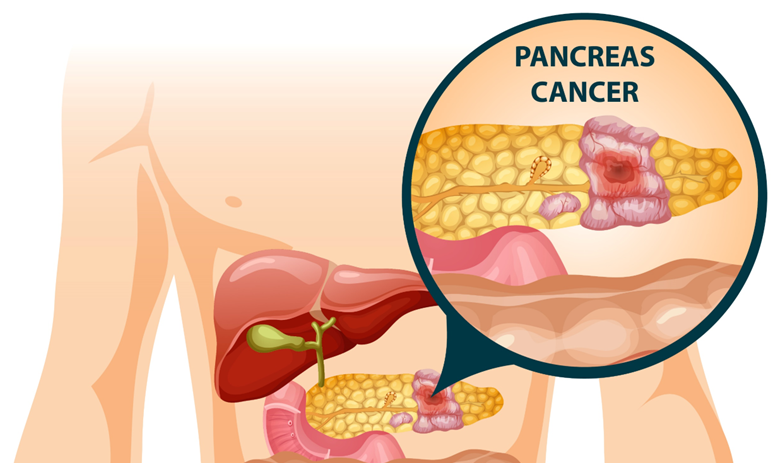
- Pancreatic Cancer: Pancreatic cancer is often diagnosed at an advanced stage, making it challenging to treat. Risk factors include smoking, family history, and certain genetic mutations.
- Cystic Fibrosis-Related Pancreatic Insufficiency: In individuals with cystic fibrosis, thick and sticky mucus can block the pancreatic ducts, leading to insufficient release of digestive enzymes. This can result in malabsorption and malnutrition.
- Pancreatic Cysts: Fluid-filled sacs can develop in the pancreas. While some are benign, others may become cancerous or cause complications.
- Pancreatic Neuroendocrine Tumours (PNETs): Tumours arise from the endocrine cells of the pancreas. These can be non-functional or functional, producing hormones that cause specific symptoms.
- Hereditary Pancreatitis: A rare genetic condition that predisposes individuals to recurrent episodes of acute pancreatitis.
- Autoimmune Pancreatitis: An immune system disorder where the immune cells mistakenly attack the pancreas, leading to inflammation and scarring.
- Pancreas Divisum: A congenital condition where the pancreatic ducts fail to fuse properly during development, potentially leading to recurrent pancreatitis.
- Annular Pancreas: A rare congenital anomaly where a ring of pancreatic tissue surrounds the duodenum, potentially causing obstruction.
It’s important to note that pancreatic diseases can have varying degrees of severity, and early detection is often crucial for effective treatment. Symptoms such as abdominal pain, changes in digestion, and unexplained weight loss should prompt medical evaluation. Treatment approaches may include medication, surgery, lifestyle modifications, and, in some cases, supportive care to manage symptoms and complications.
HEALTHY PANCREAS
Maintaining a healthy lifestyle can contribute to the well-being of your pancreas and reduce the risk of certain pancreatic diseases. Here are some practices to support pancreatic health:
- Balanced Diet: Eat a well-balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the consumption of processed foods, sugary beverages, and excessive amounts of saturated and trans fats.
- Maintain a Healthy Weight: Achieve and maintain a healthy weight through a combination of a balanced diet and regular physical activity. Obesity is a risk factor for conditions like diabetes and pancreatitis.
- Regular Exercise: Engage in regular physical activity, as exercise can contribute to weight management and promote overall metabolic health. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Limit Alcohol Consumption: If you choose to drink alcohol, do so in moderation. Excessive alcohol consumption is a risk factor for pancreatitis.
- Stay Hydrated: Drink an adequate amount of water throughout the day to support overall health, including proper digestion.
- Quit Smoking: Smoking is a significant risk factor for pancreatic cancer and other pancreatic diseases. Quitting smoking can have immediate and long-term health benefits.
- Limit Processed Meats: Reduce the intake of processed meats, as they may be linked to an increased risk of pancreatic cancer.
- Manage Chronic Conditions: Effectively manage conditions like diabetes, as poorly controlled blood sugar levels can impact pancreatic health.
- Avoid Excessive Sugar Intake: Be mindful of your sugar intake, as excessive sugar consumption may contribute to insulin resistance and metabolic issues.
- Regular Health Check-ups: Schedule regular check-ups with your healthcare provider to monitor overall health, including blood sugar levels, cholesterol, and other metabolic markers.
- Manage Stress: Practice stress-reducing techniques such as mindfulness, meditation, or yoga to promote overall well-being.
- Limit Exposure to Environmental Toxins: Minimize exposure to environmental toxins and chemicals that may contribute to pancreatic health concerns.
In conclusion, the pancreas, though often working behind the scenes, plays a crucial role in maintaining our metabolic balance and digestive harmony. Nurturing its health through a mindful lifestyle—embracing a balanced diet, regular exercise, and avoiding harmful habits—becomes an investment in overall well-being. As a silent yet indispensable partner in our physiological symphony, the pancreas thrives on the choices we make daily. Welcome to the exploration of pancreatic health—a journey into the heart of metabolic vitality.