Table of Contents
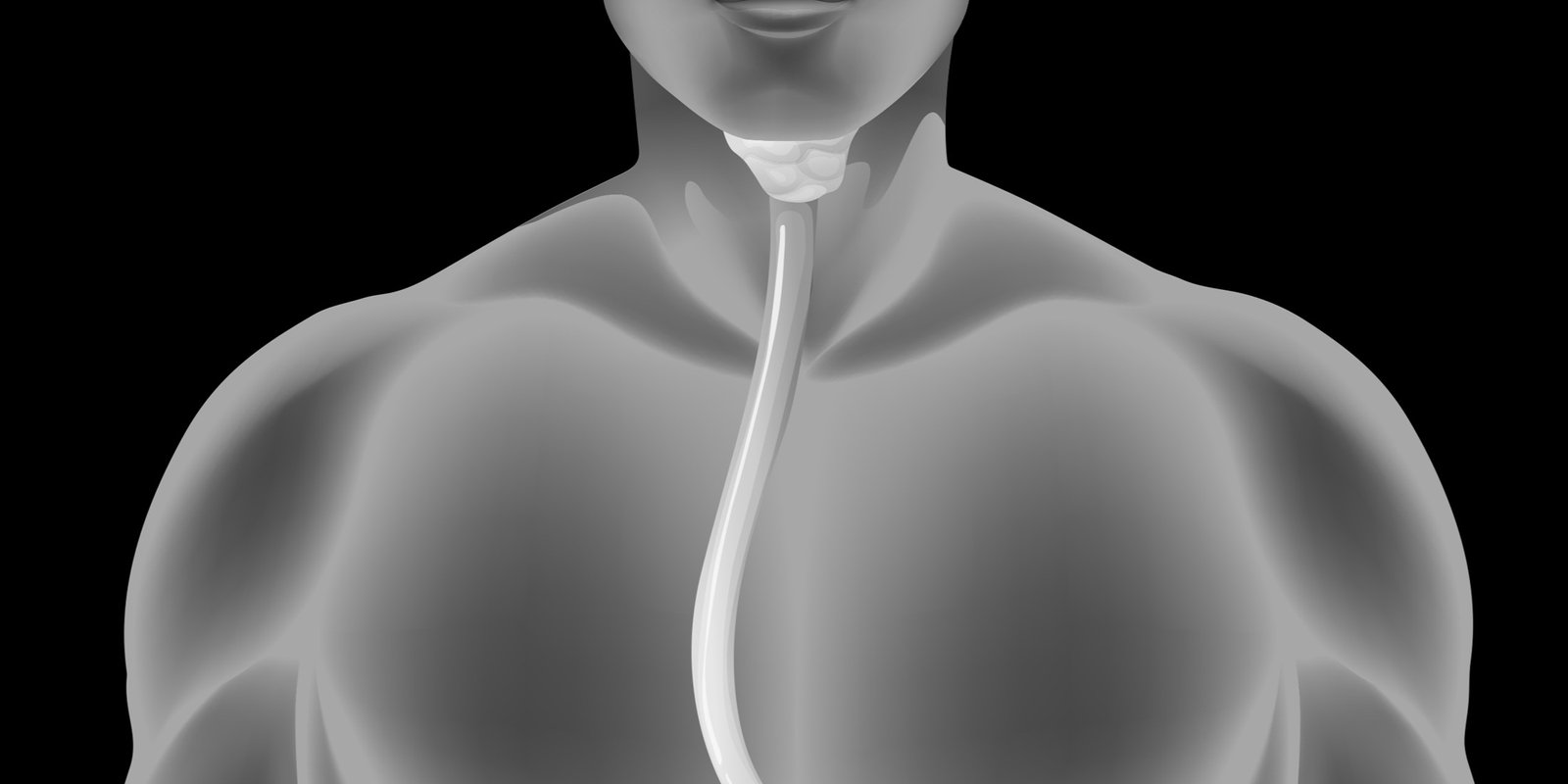
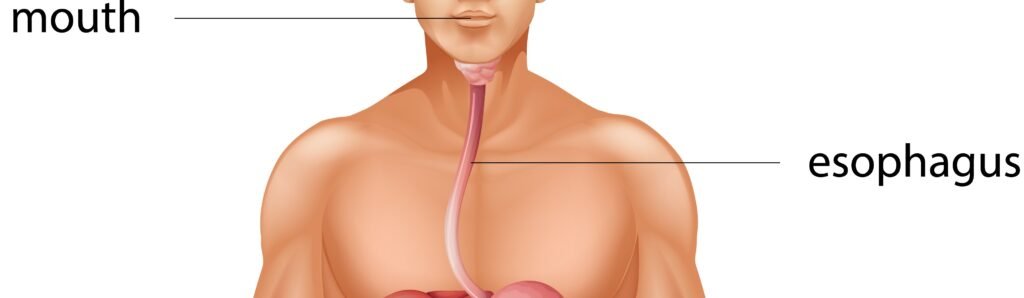
Welcome to the exploration of an essential conduit in our digestive journey—the esophagus. Often referred to as a muscular tube, the organ plays a pivotal role in transporting food and liquids from the mouth to the stomach. While its function may seem straightforward, the intricate coordination of muscles and the precision in its design contribute to seamless digestion. Join us as we embark on a fascinating journey through the anatomy, functions, and significance of the esophagus in the intricate dance of the digestive system. From the initiation of swallowing to the gentle propulsion of sustenance toward the stomach, the esophagus stands as a testament to the remarkable orchestration of the human body.
Let’s unravel the mysteries behind this seemingly simple yet indispensable part of our digestive anatomy and appreciate its role in ensuring the smooth passage of nourishment for our well-being.
ANATOMY
The esophagus is a muscular tube that facilitates the passage of food from the mouth to the stomach during the process of swallowing. This vital organ is part of the digestive system and consists of several anatomical features that contribute to its function.
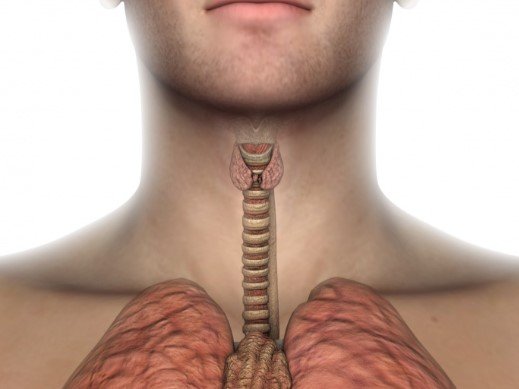
This organ extends from the pharynx to the stomach and is approximately 25 centimeters (10 inches) in length. It is located posterior to the trachea and passes through the diaphragm before connecting to the stomach.
The wall of the esophagus is composed of four main layers. The innermost layer, the mucosa, is lined with stratified squamous epithelium, which protects against abrasion from ingested food. Beneath the mucosa is the submucosa, which contains blood vessels, nerves, and glands that secrete mucus. The muscularis externa is responsible for peristalsis, the rhythmic contractions that propel food through the esophagus. The outermost layer, the adventitia, is a connective tissue layer that surrounds the organ.
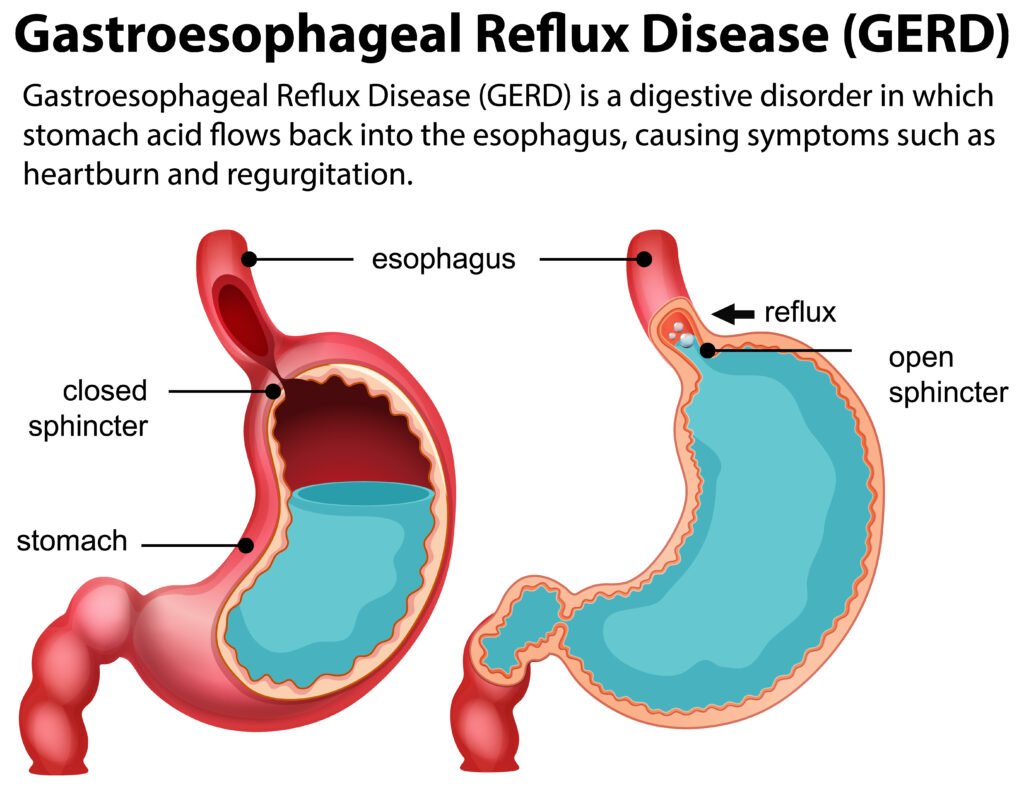
The upper esophageal sphincter (UES) and the lower esophageal sphincter (LES) are muscular rings that act as valves, controlling the entry and exit of food. The UES is located at the junction between the pharynx and the esophagus, while the LES is situated at the connection between the esophagus and the stomach. These sphincters prevent air from entering the organ during breathing and help prevent stomach contents from refluxing into the esophagus.
The blood supply to the pipe is primarily through branches of the thoracic aorta, including the esophageal branches of the aorta. Venous drainage occurs through esophageal veins that eventually join the azygos and hemiazygos veins.
Innervation of the esophagus is provided by the vagus nerve, a part of the autonomic nervous system. The vagus nerve controls the smooth muscle contractions and glandular secretions in the organ.
FUNCTION

The esophagus serves a crucial function in the digestive system, primarily focused on the transportation of food and liquids from the mouth to the stomach. Here are the key functions of the organ:
INGESTION
The esophagus facilitates the ingestion process by propelling ingested food from the mouth to the stomach through coordinated muscular contractions known as peristalsis. As a crucial part of the digestive system, the esophagus ensures the efficient and unidirectional transport of food, enabling the subsequent stages of digestion and nutrient absorption to take place.
SWALLOWING
Swallowing involves a coordinated sequence of muscular contractions, known as peristalsis, that moves the food bolus from the back of the mouth through the pharynx and into the esophagus. This process is essential for the safe passage of food to the stomach.
TRANSPORTATION TO THE STOMACH
The esophagus serves the vital role of transporting ingested food from the mouth to the stomach through peristaltic contractions. Its muscular walls propel the food bolus, ensuring unidirectional movement. This efficient transportation process is crucial for initiating the digestive journey, facilitating further breakdown and absorption in the stomach.
SPHINCTER CONTROL
The food pipe is equipped with two sphincters, muscular rings that control the entry and exit of substances. The upper esophageal sphincter (UES) regulates the passage of food from the pharynx into the esophagus, while the lower esophageal sphincter (LES) controls the release of material from the esophagus into the stomach.
PREVENTION OF REFLUX
The organ prevents reflux by employing muscular sphincters— the upper and lower esophageal sphincters (UES and LES). These valves act as barriers, ensuring unidirectional flow. The UES guards against air entry, while the LES prevents stomach contents from refluxing into the esophagus, safeguarding against conditions like gastroesophageal reflux disease (GERD).
MUCOUS SECRETION
The esophagus secretes mucus through its submucosal glands, contributing to lubrication and protection. This mucous layer helps reduce friction during peristalsis, facilitating the smooth passage of ingested food. Additionally, it acts as a safeguard, shielding the esophageal lining from potential irritation caused by acidic or abrasive substances.
TRANSPORTATION OF AIR
The food pipe does not have a primary role in transporting air; its focus is on the passage of food to the stomach. However, during swallowing, the upper esophageal sphincter briefly opens to allow the passage of swallowed air into the organ, preventing air from entering the trachea and lungs.
COORDINATION WITH RESPIRATORY SYSTEM
The esophagus coordinates with the respiratory system during swallowing. The upper esophageal sphincter briefly opens, allowing the passage of swallowed air. This collaboration ensures that air enters the esophagus rather than the trachea, preventing aspiration and maintaining the separation of the digestive and respiratory pathways.
DISEASES
The esophagus can be affected by various diseases and conditions that may impact its structure and function. Here are some common diseases of the food pipe:
- Gastroesophageal Reflux Disease (GERD): GERD is a chronic condition where stomach acid regularly flows back into the organ, leading to irritation and inflammation. Persistent GERD can result in complications such as esophagitis and Barrett’s esophagus.
- Esophagitis: Esophagitis is inflammation of the esophagus, often caused by the reflux of stomach acid, infections, or certain medications. It can lead to symptoms like heartburn, chest pain, and difficulty swallowing.
- Barrett’s Esophagus: This condition is characterized by changes in the lining of the organ due to long-term exposure to stomach acid. Barrett’s esophagus is a risk factor for esophageal cancer.
- Esophageal Cancer: Esophageal cancer can develop in the lining of the esophagus. There are two main types: squamous cell carcinoma and adenocarcinoma. Risk factors include smoking, heavy alcohol consumption, and conditions like Barrett’s esophagus.
- Achalasia: Achalasia is a rare disorder characterized by the inability of the lower esophageal sphincter to relax, causing difficulty in swallowing and the accumulation of food in the esophagus.
- Esophageal Stricture: A stricture is a narrowing of the esophagus, often resulting from chronic inflammation or the formation of scar tissue. It can lead to difficulty swallowing.
- Hiatal Hernia: A hiatal hernia occurs when a portion of the stomach protrudes into the chest through the diaphragm. This can contribute to GERD and may cause symptoms like heartburn.
- Esophageal Varices: Esophageal varices are swollen veins in the lining of the esophagus, often associated with liver diseases such as cirrhosis. They can lead to serious bleeding if they rupture.
- Eosinophilic Esophagitis: This is an allergic inflammatory condition of the esophagus characterized by the presence of an elevated number of eosinophils. It can cause difficulty swallowing and food impaction.
- Diverticula: Esophageal diverticula are pouch-like protrusions that can develop in the walls of the pipe. They may cause difficulty swallowing and regurgitation of food.
- Infectious Esophagitis: Various infections, including those caused by fungi, viruses, or bacteria, can lead to inflammation of the esophagus.
It’s important to seek medical attention if you experience symptoms such as persistent heartburn, difficulty swallowing, chest pain, or unexplained weight loss, as these may indicate underlying esophageal issues. Early diagnosis and appropriate treatment are crucial in managing esophageal diseases.
HEALTHY ESOPHAGUS
Maintaining a healthy esophagus involves adopting lifestyle habits that support overall digestive health and reduce the risk of conditions such as gastroesophageal reflux disease (GERD) and esophageal cancer. Here are some tips to keep your muscular tube healthy:
- Eat a Balanced Diet: Include a variety of fruits, vegetables, whole grains, and lean proteins in your diet. A well-balanced diet provides essential nutrients and supports overall digestive health.
- Maintain a Healthy Weight: Achieve and maintain a healthy weight through a balanced diet and regular exercise. Excess weight, especially around the abdomen, can contribute to GERD and increase the risk of esophageal issues.
- Limit Acidic and Spicy Foods: Reduce the consumption of acidic and spicy foods, as they may contribute to irritation of the esophagus. Common triggers include citrus fruits, tomatoes, chocolate, and spicy dishes.
- Avoid Overeating: Practice portion control and avoid overeating. Large meals can put additional pressure on the lower esophageal sphincter (LES), potentially leading to reflux.
- Stay Hydrated: Drink an adequate amount of water throughout the day. Proper hydration helps maintain the mucous lining of the esophagus and supports overall digestive function.
- Chew Food Thoroughly: Chew your food thoroughly before swallowing. This aids in the digestive process and reduces the strain on the esophagus.
- Maintain Good Posture: Sit or stand upright while eating. Avoid lying down immediately after meals, as this can increase the risk of acid reflux.
- Limit Alcohol and Caffeine: Moderate your consumption of alcohol and caffeinated beverages. Both can relax the LES, potentially leading to reflux.
- Quit Smoking: If you smoke, consider quitting. Smoking can weaken the LES and contribute to the development of esophageal issues.
- Avoid Late-Night Eating: Allow sufficient time between your last meal and bedtime. Late-night eating can increase the likelihood of reflux.
- Manage Stress: Practice stress-reducing techniques such as deep breathing, meditation, or yoga. Stress can contribute to digestive issues, including GERD.
In conclusion, the esophagus, though often overlooked in its daily role, plays a vital part in our digestive symphony. Its health is intertwined with our overall well-being, influencing how we nourish our bodies. By embracing mindful eating habits, staying hydrated, maintaining a healthy weight, and addressing lifestyle factors, we can contribute to the resilience and vitality of this essential conduit. Remember, a healthy esophagus ensures the smooth passage of sustenance, allowing us to savour the joys of nourishment and promoting digestive harmony. Prioritizing these simple yet impactful measures is a testament to our commitment to holistic health, fostering a thriving esophagus for a healthier and more enjoyable life.